INTRODUCTION
Paroxysmal nocturnal hemoglobinuria (PNH) is a rare, acquired hematologic disease characterized by chronic complement-mediated intravascular and extravascular hemolysis. In the phase 3 PEGASUS study (NCT03500549), pegcetacoplan, a C3 inhibitor targeting the proximal complement pathway, was superior to eculizumab (ECU) on the primary endpoint of hemoglobin (Hb) change from baseline at week 16, and improved clinical and hematologic parameters. Additional analyses assessed if any groups of patients might experience further benefit from pegcetacoplan.
METHODS
Patients ≥18 years old with a diagnosis of PNH and persistent anemia (Hb <10.5 g/dL) at baseline, despite treatment with stable doses of ECU for ≥3 months, entered a 4-week run-in period during which all patients continued their current dose of ECU with the addition of twice-weekly pegcetacoplan (1080 mg, self-administered subcutaneously). On study day 1, patients were stratified based on baseline platelet count and prior transfusion requirements, and randomized 1:1 to monotherapy with pegcetacoplan or ECU for 16 weeks. The primary endpoint of change from baseline (before first dose of pegcetacoplan) at week 16 in Hb and key secondary endpoints (change from baseline at week 16 in absolute reticulocyte count [ARC] and lactate dehydrogenase [LDH]) were analyzed using a mixed-effect model for repeated measures by subgroups based on baseline age group, sex, race, number of packed red blood cell transfusions (<4 vs ≥4) within the 12 months prior to day −28, and platelet count at screening (<100,000/mm3 vs ≥100,000/mm3). The key secondary endpoint of transfusion avoidance was analyzed by calculating the number and proportion of patients who were transfusion-free and also analyzed by subgroups. For patients transfused during the randomized control period or who withdrew from the study, the primary and secondary data endpoints up to the transfusion or time of withdrawal were included, but all subsequent values were censored.
RESULTS
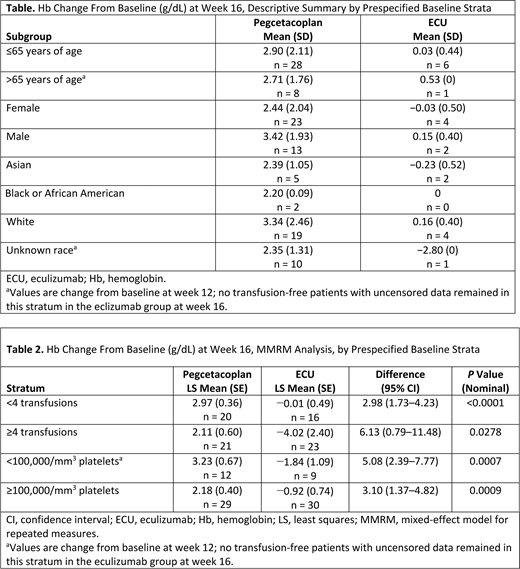
Pegcetacoplan treatment was associated with significantly greater increases in Hb levels than ECU at week 16, regardless of baseline age group, sex, race, prior transfusions, or platelet count (Tables 1-2). At week 16, regardless of baseline platelet count strata, mean Hb significantly increased from baseline in the pegcetacoplan group and decreased in the ECU group. The proportion of transfusion-free patients was similar in the pegcetacoplan group, regardless of age (≤65 years, 87.1%; >65 years, 80%), sex (female, 81.5%; male, 92.9%), race (Asian, 100%; black, 100%; white, 75.0%), transfusion strata (<4 transfusions, 85.0%; ≥4 transfusions, 85.7%), or platelet strata (<100,000/mm3, 83.3%; ≥100,000/mm3, 86.2%). A smaller proportion of patients were transfusion-free with ECU, regardless of age (≤65 years, 18.8%; >65 years, 0%), sex (female, 18.2%; male, 11.8%), race (Asian, 28.6%; black, 0%; white, 16.0%), transfusion strata (<4 transfusions, 31.3%; ≥4 transfusions, 4.3%), or platelet strata (<100,000/mm3, 0%; ≥100,000/mm3, 20.0%). Similar trends for more favorable results with pegcetacoplan versus ECU were seen across the prespecified subgroups for ARC and LDH.
CONCLUSIONS
In this prespecified stratified analysis of the phase 3 PEGASUS study of patients with PNH and persistent anemia, mean Hb levels increased significantly more, the proportion of transfusion-free patients was significantly higher, ARC change from baseline at week 16 was significantly lower, and LDH decreases were larger with pegcetacoplan versus ECU, regardless of baseline age group, sex, race, prior transfusion numbers, and platelet count.
Peffault De Latour:Pfizer: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Alexion Pharmaceuticals Inc.: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Amgen: Research Funding; Apellis: Membership on an entity's Board of Directors or advisory committees. de Castro:Alexion: Honoraria, Research Funding; Apellis: Consultancy, Honoraria, Research Funding; Novartis: Honoraria, Other: Steering committee; Biocryst: Honoraria, Other: Data monitoring committee. Szer:Apellis: Consultancy; Pfizer: Honoraria, Speakers Bureau; Novartis: Consultancy, Honoraria, Speakers Bureau; Alexion Pharmaceuticals Inc.: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Takeda: Honoraria, Speakers Bureau; Prevail Therapeutics: Honoraria, Membership on an entity's Board of Directors or advisory committees. Usuki:Alexion: Research Funding, Speakers Bureau; Apellis: Research Funding; Chugai: Research Funding; Novartis: Research Funding, Speakers Bureau. Hillmen:Alexion: Consultancy, Research Funding, Speakers Bureau; Apellis: Consultancy, Research Funding, Speakers Bureau; Gilead: Other: Financial or material support, Research Funding; AstraZeneca: Consultancy, Speakers Bureau; Roche: Consultancy, Other: Financial or material support, Research Funding, Speakers Bureau; AbbVie: Consultancy, Other: Financial or material support, Research Funding, Speakers Bureau; Pharmacyclics: Other: Financial or material support, Research Funding; Janssen: Consultancy, Other: Financial or material support, Research Funding, Speakers Bureau; Acerta: Other: Financial or material support. Griffin:Alexion Pharmaceuticals: Honoraria, Other: Conference Support; Biocryst: Membership on an entity's Board of Directors or advisory committees. Hamdani:Apellis Pharmaceuticals: Current Employment, Current equity holder in publicly-traded company. Ajayi:Apellis Pharmaceuticals: Current Employment, Current equity holder in publicly-traded company. Weitz:Alexion: Consultancy, Honoraria, Speakers Bureau; Apellis: Consultancy, Honoraria.
Pegcetacoplan is an investigational drug for the treatment of paroxysmal nocturnal hemoglobinuria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal